Where We Work
See our interactive map


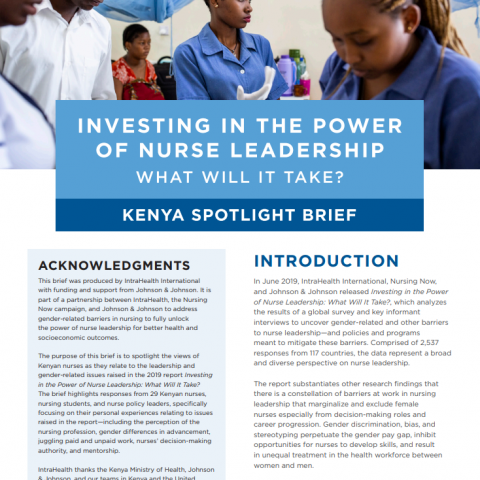
Mary is the deputy nursing officer at the Lodwar County Referral Hospital in Turkana County, Kenya. Photo by Patrick Meinhardt for IntraHealth International.
I don’t think nursing is a job that is coveted by many, but to me, it's a calling.
Mary Akai Supat is the deputy nursing officer at the Lodwar County Referral Hospital in Turkana County, Kenya. She’s in charge of 50 people and three departments: Accident and Emergency, Critical Care, and Maternal and Child Health. We first met her when she participated in a training conducted by our USAID-funded Human Resources for Health (HRH) Kenya Program on long-acting reversible family planning methods. Last February, we sat down to talk to her about her experiences as a nurse.
This piece is part of our special content series, Nurse Leadership: In Their Own Words.
I graduated [from nursing school] in 2003 and I had been working for nonprofit organizations for a long time before I joined the Ministry of Health. To me, it is a calling, I felt like being a nurse starting from the word “go” when I was growing. I loved taking care of the sick, I loved helping the needy.

Her facility delivers babies like this one, who was meeting their grandmother for the first time. Photo by Patrick Meinhardt for IntraHealth International.
I'm a Turkana [an ethnic group native to Turkana County in Kenya] by origin. When I first started nursing, I had small kids that kept me around here. I wanted to see them grow. It was a bit hectic because the facilities I was working with were not baby friendly. So, at times I'd leave my child a whole day without breastfeeding. When I came home, my child would cry a lot because she had not had enough milk. It wasn't easy.
The community here does not allow parents to share childcare duties. Child bearing, child caring, and child upbringing is meant for the mother. It is not a shared responsibility. It's solely for the mother to do all that.
A house help eventually helped care for my children while I was at work. If you're not able to afford a house help, another alternative would be to take your child to your mother. But generally nurses take care of their children or you hire a house help to take care of your child.

She knows that her colleagues have to support each other for the health facility to be successful.
As nurses, we all support each other. Like, my colleague Rebecca has a young child, so she reports in the morning at around 10:00 am and then we allow her to go breastfeed for an hour. Her case now is different, unlike when I was taking care of my children.
Then in the afternoon we cover for her so that she can have enough time with her child. But this is only until she weans, then she will come back full-time.
We support one another, because tomorrow it will be me. I'll need her support, and the other day it will be you and you'll need our support.

But nursing is a challenge, especially because it comes with a lot of responsibilities.
I don’t think nursing is a job that is coveted by many because it comes with a lot of responsibilities. Like if you asked me today if I receive anything extra on top of my ordinary pay because of this position, I would tell you no.
In our case here, we don't have a nursing directorate in this county. So we find it challenging to articulate nursing issues, because we are placed under another directorate, like a medical service directorate. So we receive very little support and are not allowed to make our own decisions.
We are here because we are nurses—we are human. Nursing is a calling. It is what I love to do. Otherwise, there's nothing motivating me to be in this position.

Alice feels like it's an uphill task to be a nursing officer in charge in such an era.
If we had our own directorate, things would be different. It is an uphill task to be a nursing officer in charge in such an era.
We don't have a [nursing] budget so we can’t budget for our own things or make budgetary decisions. I wish I had a working computer, for example. I have a desktop that is not operational. I keep writing hard copies, yet we are in the IT era. I'm supposed to have teleconferences but for us a working network is still a big challenge. Yet we're supposed to be at the same level with the rest of the world. We're supposed to give the same care. We cannot.

Nurses sometimes feel they are perceived as competitors by other health workers.
The challenge is that there are laws that bar the nurses from certain things. And there are perceptions about us. Doctors, for example, they always perceive nurses as competitors. To me that is because the other professions, like medicine, perceive that nurses will outgrow and outshine them.
Everybody guards their territory. They say, “Don’t encroach, you're a sister nurse, you be there.”

But it's worth it to change lives, like lowering the neonatal death rate.
Last year, I attended a neonatal conference that was held in Nairobi. From the knowledge I gained there, I was able to overhaul the whole unit. We changed the set-up for the newborn babies and separated the premature babies. That was all targeted to minimize the neonatal deaths that were occurring due to sepsis. Before, the babies who were born at home when they're sick used to be placed in the same place as those that were born in the hospital. To me it was a big achievement. Even now as we talk of a lower death rate, I'm glad that I was able to attend.

Nurses do everything, but the pay does not relate to the number of hours you work.
There is an imbalance in terms of promotion. You'll find somebody recently employed was promoted based on who they know, and so many other things. Unlike before [devolution], when the government used to promote everybody after three years.
Then there is also another discrepancy. A doctor who is a graduate is not employed the same way a graduate nurse is. So nursing is still deemed as a lower profession compared to medicine. Plus, nurses don't get the same benefits.
A medical officer will start with a higher job group than the nurse and only comes to see a patient to conduct rounds. It is the nurse who cleans the patient. It is the nurse who gives them medicine. It is the nurse who is on night duties, who spends time with the patient. The nurse literally is always with the patient. The pay does not relate to the number of hours you're working.

To their communities, nurses mean everything.
But we know that the community’s perception of a nurse is very positive. They know even back in the village that the nurse is everything. The nurse does everything, literally everything, because nurses are the ones who run the small dispensaries and health facilities down there in the village. You will not find a doctor there, neither will you find a clinical officer. You'll always find a nurse.
Of course, because it is the nurse who will conduct the delivery. It is the nurse who will tie or who will dress that wound. It is the nurse who will refer that patient. So to them, the nurse is all around. The nurse means everything to them.
READ what nurses in Kenya say about leadership and gender-related issues in Investing in the Power of Nurse Leadership: Kenya Spotlight Brief.
Carol Bales and Samantha Rick, former IntraHealth staff/consultant, interviewed Mary Akai Supat just before the COVID-19 pandemic lock down. Katherine Seaton edited Mary’s interview for clarity and length. All photos by Patrick Meinhardt for IntraHealth International. All work related to this post and the Kenya brief was funded by a grant from Johnson & Johnson Foundation.
Get the latest updates from the blog and eNews
Read what nurses in Kenya say about nursing leadership in Investing in the Power of Nurse Leadership: Kenya Spotlight Brief. Twenty-nine nurses, nursing students, and nurse policy leaders shared their personal experiences including gender differences in advancement, juggling paid and unpaid work, decision-making authority, and mentorship.